If you're wondering whether your poor sleep quality is connected to your POTS, you're in the right place. In this article, we'll explore how dysautonomia affects your sleep—and how poor sleep, in turn, worsens autonomic dysfunction. It's a bit of a vicious cycle.
One of the first questions I ask my patients with dysautonomia is: How is your sleep?
-
How many hours do you get?
-
Do you feel rested when you wake up?
-
Are you a light sleeper? A heavy one?
-
Is getting out of bed in the morning a battle?
These questions offer important insight into how much POTS may be interfering with your rest. Poor sleep means poor recovery—from exercise, from stress, and especially from POTS flares. It also tells me how to adjust your cardiovascular rehab plan. So… what's the cause?
There are many theories explaining why dysautonomia disrupts sleep, but one of the most compelling and understandable answers is cortisol.
Cortisol: A Toxic Relationship
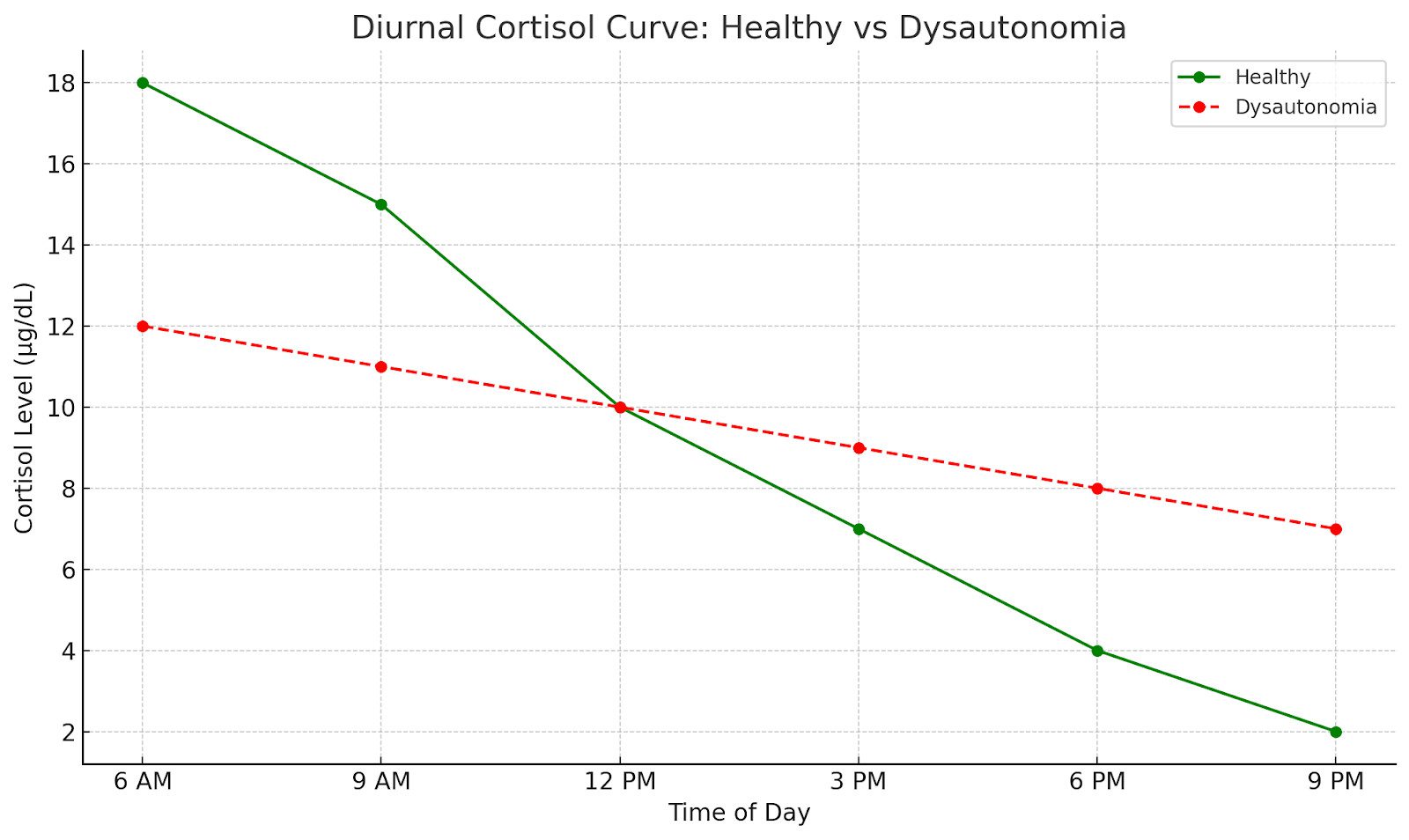
Cortisol is your body's primary stress hormone. It governs your "fight or flight" response, but it also plays a vital role in keeping you alert, energized, and functioning. Ideally, cortisol peaks in the morning (to help you feel awake) and tapers off throughout the day (so you can wind down and sleep at night).
But in patients with POTS, this rhythm is disrupted.
As you can see in the graph above, people with POTS do experience a cortisol rise in the morning—but it's often weaker than that of healthy individuals. Even worse, cortisol tends to stay elevated throughout the day and into the evening, when it should be falling. So not only do you wake up feeling groggy (because your cortisol didn't spike properly), but you're also wired and restless at night (because it didn't drop).
It's like being stuck in a toxic relationship with your hormones—when you need them most, they're nowhere to be found; when you need peace and quiet, they're loud and needy.
So… How Do We Fix the Relationship?
You and cortisol need a bit of couples counseling. Here are three key interventions I've found helpful for my patients:
1. Wake up at the same time every day—no matter what.
This is a battle, especially when the snooze button feels ecstasy to someone with POTS. But snoozing teaches your body not to expect cortisol in the morning. Over time, this flattens your natural rhythm and makes mornings even harder. Sticking to a consistent wake-up time helps signal to your body: "Hey, this is when I need that energy."
2. Meditation or mindfulness practice.
I know—most POTS patients who've tried meditation feel like they failed. That's normal. With elevated cortisol, the mind can be hard to calm. But learning to meditate is a process—it takes time, and the benefits build slowly. Meditation is one of the few tools we have that directly reduces cortisol and helps reset your nervous system. Meditation for POTS is a whole other article for another day. Just don't give up on that endeavor. Meditation throughout the day can help lower this average cortisol levels letting cortisol know, hey you don't need to follow me around all day, I got this.
3. Lights out = cortisol out.
No lights, no screens, and nothing stimulating before bed. Even though your phone feels like a wind-down tool, the light tells your brain it's still "go time." This keeps cortisol elevated just when you want it to fade. A calm, dark evening routine helps cue your body that it's time to rest and reset. This tells cortisol, hey now is not the right time Dr. Fox says you are being a little "co-dependent."
Be Patient—It's a Long Game
These changes won't yield results in a day. If we could cure insomnia in one night without medication, no one would be on sleep aids. But if you stick with these habits—consistent wake time, mindfulness, and proper wind-down—you'll likely begin to see deeper, more restorative sleep, better recovery, and fewer symptoms over time.
Healing your relationship with cortisol is one of the most impactful steps you can take to manage dysautonomia—and sleep is the gateway.