The following is an interview with Dr. Nathan Yokel, Physician at Regenerative Orthopedic and Sports Medicine located in Washington, DC and Northern Virginia area. We will discuss Platelet-Rich Plasma (PRP) and regenerative medicine and get a deeper insight on this emerging field of medicine.
Chris: What is it that you do and what is PRP (platelet-rich plasma), and what is the difference between PRP (platelet-rich plasma) and prolotherapy?
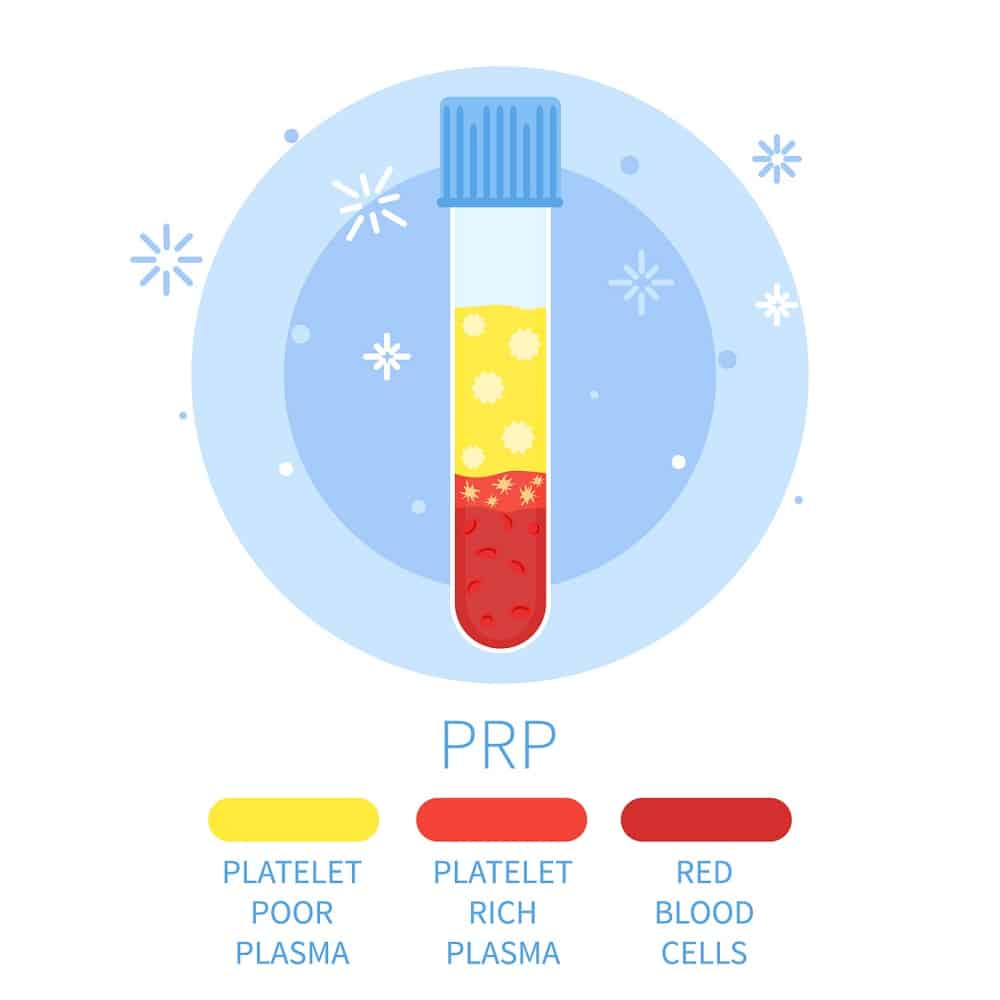
Dr. Yokel: When I look at a patient, as a physiatrist I focus on the breakdown and the mechanics that leads to the injury. I do a complete physical exam, and confirm the findings with diagnostic ultrasound. When ready to start thinking about treatment, that’s when prolotherapy is considered. Prolotherapy, which is short for proliferative therapy, is when you inject any kind of substance from outside the body to inside the body to cause this “proliferative” reaction. It causes an inflammatory cascade, and drives a lot of the inflammatory mediators and growth factors to the areas that we inject. These treatments have been around for many many years but more so popularized recently. Under a diagnostic ultrasound, we use a dextrose or a sugar solution and dilute it in lidocaine and saline. We then inject it into the body to cause this proliferative reaction. The difference between prolotherapy and the PRP or the (Platelet-rich plasma) is with PRP we are taking the patients’ blood placing it in a centrifuge it to isolate different layers of the blood and taking the platelet rich portion and injecting them back into the body to have both a direct concentrated effect and the secondary inflammatory reaction. There are many more regenerative treatments out there that we perform, for example, “amniotic membrane treatments” and various other stem-cell treatments that are becoming more and more popular and continuing to progress.
Chris: How would a person know if a treatment like this would be beneficial to them?
Dr. Yokel: It starts by trying to figure out what the problem is. It is mainly diagnosing not only what the acute problem is, but what was the breakdown in biomechanics that led to this problem. As far as trying to figure out what is the best treatment for you, it’s not always the same for every person or condition. The foundation for our treatment is getting that patient in with a good physical therapist and work on some of these strength and activation patterns to develop a good way to rest the area as needed and remove tension to heal naturally to prepare them for these regenerative treatments. Specifically, when trying to figure out when to use prolotherapy, or any of these regenerative treatments, that depends on the condition. If it is a small tendon tear, or an area of irritation within a ligament, and an area with relatively good blood flow, this might be a good choice for prolotherapy. If it’s a larger tear with not the greatest blood flow like the base of a meniscus, then it may be something that is better treated with platelet rich plasma treatment. Large gap tears that require scaffolding, end stage or moderate arthritis that require some cartilage regrowth this may require a stem cell based treatment.
Chris: So, people who have been told that they may require total knee replacements or shoulder reconstruction, could something like PRP (Platelet-Rich Plasma) could be beneficial for them?
Dr. Yokel: Yes, I believe it’s all in diagnosing what the true problem is. If you’ve had arthritis in your knees for 20 years and then over the last 3 months you have worsening pain, chances are it’s not the arthritis that’s causing the problem it’s the meniscus injury that’s already been degenerative and it put you over the edge. The goals for these regenerative treatments in that instance is not to turn the clock back 20 years but to turn the clock back 6 months when things were pretty well. Doesn’t mean the arthritis is gone but you really stabilized the pain generators. A lot of these patients would really benefit from learning about their body. Working on the strength patterns with a physical therapist or doing some exercises to give themselves a better foundation for success. If they are much stronger going in to get the knee replacement they will have a better outcome with the actual procedure.
Chris: Is there evidence for these types of treatments? There seems to be conflicting evidence and research. What is your perspective on this?
Dr. Yokel: I believe that the literature can be a hit or miss. Part of that is because a lot of these studies for the PRP (Platelet-Rich Plasma) and regenerative treatments are self-funded, meaning they are done by a physician or they are done by a hospital group that’s trying to investigate the process. They are not funded by a large scale pharmaceutical company and because of that sometimes the numbers are not as great. Its’s a very difficult type of treatment to do a placebo controlled double randomized blinded study. What we are left with is a large amount of smaller case series and smaller studies where some patients received the treatments and others didn’t. However, it’s hard to match the treatments because of the variable degree of injuries. Two people may have meniscal tears but not the exact type and same goes for rotator cuff tears. For me the turning point is trying to figure out what all the options are for patients, which option is the least invasive and has the biggest chance for success. We then list the benefits and to try and decide which is best for treatment. I am a strong believer that these treatments work and that in time more evidence will play out of it. The question is, what will it take to tip it over the edge to the point where it becomes a more accepted procedure? Also, what will it take for the insurances to approve these procedures? I would encourage the people looking for information on these procedures to look at the research that is out these on the internet and look for clearing houses or articles.
Chris: Is there some research out on particular injuries and treatments that there are more studies on?
Dr. Yokel: Yes, but again Its kind of difficult to gage. Some of the most common areas that we have strong treatment experiments for are: rotator cuff injuries, meniscal injuries, and other common injuries like tennis elbow. With prolotherapy, there is a lot of evidence for using it to treat mild to moderate knee arthritis. One website out there that’s kind of a clearing house on prolotherapy research that I would recommend is on our website WWW.ROSM.ORG by Dr. Dean Reeves. This website has a clearing house of prolotherapy research from over the years categorized by different body parts and conditions that can be very helpful.
Chris: What is the role of physical therapy, post PRP (Platelet-Rich Plasma) and post regenerative treatment, in terms of getting people back to where they should be and working in conjunction with physiatrists like yourself?
Dr. Yokel: I think the reason that we get a lot of our best results is because we work closely with a physical therapist. I think if you tell someone that you need to rest that area for a week or two and then get back at it, but you don’t give them the guidance as far as how to ease back into things, you are setting them up for a non-optical outcome or re injury. So, part of where the role of a physical therapist comes in is whenever I see my patients I give them a very detailed physical therapy prescription that tells the therapist of exactly what I think is going on. When we are working with the therapists we really want to make sure that we are teaching the patient the exercises that they can do, not just to solve the acute issue, but to make sure that it doesn’t come back again. Specifically, after the regenerative treatments sometimes I will tell a patient to take a few days off from therapy and really rest the area and then go back to see your therapist. Sometimes we will give the therapist a post treatment protocol that tells them what to do during each phase of healing. I really encourage patients to work with a physical therapist. I think in general a lot of times the therapist have the richest insight to a lot of their patients because they spend a lot of time with them during the week and in their ear about what they need to do to get out of this problem.
Chris: When someone has an injury and they are told by a doctor that surgery is the only option however, insurance may cover surgery but not the regenerative treatments, what may be your approach to counseling the patient to make the best decision of regenerative treatment VS. Surgery?
Dr. Yokel: The first thing I would say to any patient out there is to see another surgeon and get a second opinion to make sure two like-minded experts agree and figure out the different possible approaches and outcomes. Specifically, from patient to patient I think the best thing you can try and do is gather more information to help you make the decision. You can do this by getting opinions from different surgeons, or even speaking to you therapist who knows you and your body well or getting an opinion from a non-surgical perspective. You have to factor in recovery time post-surgery, impact on life style that a more invasive procedure may have when weighing out the two.
Chris: Is all PRP and prolotherapy created equal? Why is it so important to do it under ultrasound?
Dr Yokel: There is a huge discussion within the regenerative community as to what should be allowed to be called PRP. There are such variables within the concentration of platelets and the purity. There is a slew of companies that make these kits for processing the Platelet-Rich Plasma (PRP). With prolotherapy you can do different degrees of concentration with the prolotherapy solution and that can have a huge effect on the amount of inflammation that it causes. For these regenerative treatments, it is definitely less effective if you do free hand procedures and if you don’t get it in the right spot it won’t be nearly as potent. For me I think trying to decide between microscopic and ultrasound guides, is night and day as far as the detail you can see. By using ultrasound guides you can see that little tear in the ligament where you see that defect and can watch the needle go in there and watch the treatment go in there to know that you hit the right spot.