Patients often report an increase in loss of balance events or falls following a cancer diagnosis.
According to a 2002 article(1), this increased risk comes from several factors, including impaired physical function, neurological deficits, use of multiple medications, deconditioning, and treatment-related fatigue.
In this blog, we will discuss how those factors can impair balance and contribute to fall prevalence, as well as how physical therapy can help reduce or eliminate these symptoms.
1. Neurological Deficits
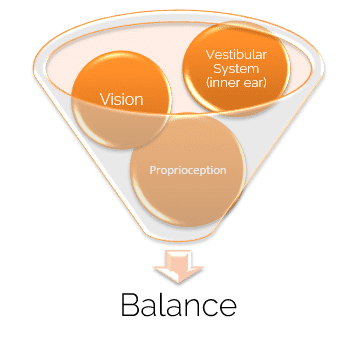 The three neurological systems that influence balance are vision, proprioception (pressure, touch, and joint position), and the vestibular system (inner ear).
The three neurological systems that influence balance are vision, proprioception (pressure, touch, and joint position), and the vestibular system (inner ear).
A class of symptoms, called paraneoplastic neurologic syndromes (2) occur as an inflammatory response caused by cancer and some cancer treatments. These can affect neural transmission of sensory information, and therefore affect balance.
2. Multiple Medication Usage
A 2006 study(3) found that simultaneous use of multiple medications (polypharmacy) is correlated with an increased risk of falls.
Diuretics and medications that target the central nervous system are often prescribed to patients with cancer to reduce disease-related inflammation. CNS-targeting medications are prescribed to treat an array of other side effects. Both have the potential to affect balance and increase the risk of falling.
3. Treatment-Related Fatigue
Some side effects of cancer, including inflammation, can result in patient's fatigue. When the cancer targets large organs, the body has to work harder to maintain homeostasis, which also leads to extreme tiredness. Further, patients undergoing chemotherapy often experience chronic fatigue, and it is suggested that managing other side effects such as nausea, weakness, and pain can reduce fatigue symptoms. (4).
Physical Therapy & Fall Prevention for Patients with a Cancer Diagnosis
Physical therapy can be an effective treatment for balance dysfunction and higher fall risks for patients with cancer. By implementing a strengthening protocol, the muscles in the feet, legs, and hips will start working more efficiently, and stimulating the sensory receptors will help mitigate neurological deficits.
Although multiple medication disorders are outside the physical therapy scope of practice, your physical therapist can talk with your physician to ensure the medications are not further inhibiting balance. Finally, strengthening and implementing cardiovascular workouts will help to improve function, so the body is not working as much when at rest.
References
- Holley, S. (2002). A look at the problem of falls among people with cancer.Clinical Journal of Oncology Nursing,6(4).
- Honnorat, J., & Antoine, J. C. (2007). Paraneoplastic neurological syndromes.Orphanet journal of rare diseases, 2(1), 22.
- Ziere, G., Dieleman, J. P., Hofman, A., Pols, H. A., Van Der Cammen, T. J. M., & Stricker, B. H. (2006). Polypharmacy and falls in the middle age and elderly population.British journal of clinical pharmacology, 61(2), 218-223.
- Jacobsen, P. B., Hann, D. M., Azzarello, L. M., Horton, J., Balducci, L., & Lyman, G. H. (1999). Fatigue in women receiving adjuvant chemotherapy for breast cancer: characteristics, course, and correlates.Journal of pain and symptom management, 18(4), 233-242.





